22/11/2024
Female hormones are like the conductors of a symphony in your body, influencing everything from mood and weight to fertility. When these conductors go off-key or you have a hormone imbalance it can affect how you feel and your overall health. In this article, we’ll take a closer look at what female hormone testing can tell us– how it works, why it matters, and how it can guide you towards a healthier life.
Reproductive health
The female body is capable of a vast array of wonderful things, not least, the ability to create small humans. As you can imagine, this is an incredibly complex process involving many pathways and hormones. Here are a few of the most important female hormones to keep tabs on:
Oestradiol
Oestradiol is a form of oestrogen used to assess female reproductive function, among other things. It is crucial for the development of secondary female sex characteristics; those which develop during puberty like breast growth and the widening of the hips to name a few. Oestradiol levels decline with age. This decline is associated with elevated risk of cardiovascular complications, cognitive impairment, and osteoporosis. Finally, elevated levels of oestradiol, particularly in postmenopausal women, are associated with increased risk of breast cancer1.
Progesterone
Progesterone is a hormone essential for priming the uterus for pregnancy and supporting its maintenance during pregnancy. Therefore, it is involved in the menstrual cycle, which we will discuss in the next section. Progesterone levels can be expected to rise during the second half of your menstrual cycle and decline if pregnancy does not occur2.
Follicle Stimulating Hormone (FSH)
Growth and development of ovarian follicles is essential to pregnancy. Follicle-stimulating hormone (FSH) plays a crucial role in this process and is charged with the successful release of an egg from the ovary during ovulation. Like many of the hormones we’ll discuss, FSH levels fluctuate during the menstrual cycle, displaying the highest levels during the follicular phase. Luteinising hormone (LH) is closely related to FSH. They work together to regulate ovulation as well as menstruation. LH levels spike prior to ovulation, initiating the release of an egg from the ovary2.
Prolactin

The final hormone to consider here is prolactin. This hormone is primarily associated with lactation and milk production in women but is also involved in breast development during pregnancy and in processes surrounding breastfeeding. If you have high levels of prolactin, you may experience interference with your ovulatory and menstrual cycles, which can progress to fertility complications2.
Menstrual Cycle and Hormone Imbalance
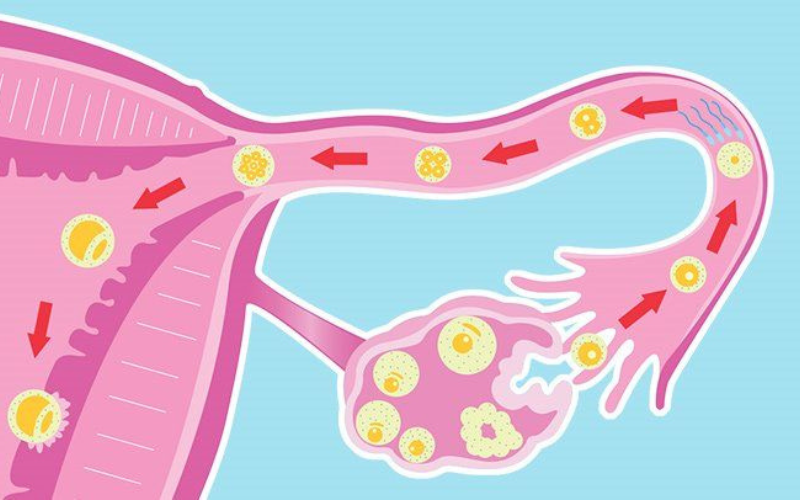
It goes without saying that a healthy reproductive system and a healthy menstrual cycle go hand-in-hand. It is therefore no surprise that the female hormones involved in these processes are similar. Oestradiol is again a crucial component in the regulation of menstruation. You can expect to see increases in oestradiol during the follicle phase and a subsequent decline during the luteal phase. Progesterone is also involved in the regulation of menstruation and the preparation of the uterus for implantation. Progesterone levels increase after ovulation and remain elevated throughout the luteal phase of menstruation3.
FSH and LH levels fluctuate throughout the menstrual cycle. FSH levels increase during the follicular phase4 and LH levels can be expected to spike just before ovulation5. Monitoring of these female hormones can help in family planning and help identify issues in your reproductive and menstrual processes.
Menopause
Menopause marks a natural and inevitable phase in a woman’s life, typically occurring between the ages of 45 and 55. During this transition, the ovaries gradually produce fewer female hormones, leading to the cessation of menstrual cycles and a decline in fertility6.
A decline in oestradiol and progesterone levels is responsible for the symptoms associated with menopause including hot flashes, vaginal dryness, and mood changes. This decline is associated with increased risk of cardiovascular disease (CVD) and osteoporosis. Prolactin levels may also decrease during menopause contributing to vaginal dryness and breast tenderness. FSH and LH are common markers for menopause. As the ovaries produce less oestrogen and progesterone, levels of FSH and LH increase, providing a method of detecting the onset of menopause6.
Testosterone is more often thought of as a male hormone. However, it is essential in the female body too. Testosterone acts as a precursor for oestrogen and has effects on most vital organ systems. It also exerts a significant influence on libido, making it a common hormone replacement therapy (HRT) for postmenopausal women7.
Sex-hormone binding globulin (SHBG) is a glycoprotein responsible for the regulation of sex hormones, acting as a hormonal transporter it influences a variety of target tissues. Levels of SHBG are known to decrease in line with menopause, which can lead to the decline of other hormones, such as testosterone6.
Hormone Imbalance and Related Health Concerns
A hormonal imbalance can disrupt your body’s symphony, which can give rise to troublesome conditions. These influential messengers dictate functions from metabolism to mood. When excess or scarcity strikes, chaos ensues, upending the rhythm of normal processes.
The most obvious is infertility. Infertility affects as many as 1 in 8 women and it’s on the rise8. Hormone imbalance in progesterone, FSH, LH and prolactin may lead to fertility complications as well as pregnancy complications such as miscarriage or preterm birth9. As we mentioned, low oestradiol is associated with increased risk for CVD and osteoporosis in older populations and increased levels may be associated with increased risk of breast or endometrial cancer9. High levels of LH are associated with polycystic ovary syndrome (PCOS), a condition with painful symptoms. Finally, SHBG has been associated with several conditions including PCOS, hypothyroidism, obesity, hirsutism (excessive hair growth), alopecia (hair loss from the scalp or other parts of the body) and acromegaly (overgrowth of bones and tissues, particularly in the hands, feet, and face)9.
Lifestyle and Your Hormonal Health
Lifestyle factors such as diet and exercise play a pivotal role in orchestrating the delicate balance of hormones. When this balance falters, it can trigger a series of health concerns and distressing symptoms. Yet, the silver lining resides in the potential of lifestyle adjustments to help recalibrate this intricate symphony10.
Oestradiol, a cornerstone of feminine vitality, responds favourably to regular exercise and the incorporation of phytoestrogen-rich foods like soy into the diet. Similarly, progesterone’s equilibrium finds support through an active lifestyle and dietary inclusion of vitamin B6. The balance of FSH can be nurtured by a combination of physical activity and the integration of omega-3 fatty acids10.
LH harmonisation can be aided with both exercise and adequate vitamin D intake. Prolactin, a critical player in lactation and reproductive health, benefits from exercise and a diet enriched with vitamin B6. The intricate partnership between free and total testosterone, guardians of strength and vitality, thrives on the twin pillars of exercise and a diet rich in nourishing proteins and healthy fats10.
Put simply, the blend of lifestyle choices and hormonal well-being takes on a crucial role. Regular exercise and thoughtful dietary choices play their part, providing potential advantages to important biomarkers like oestradiol, progesterone, FSH, LH, prolactin, free and total testosterone, and SHBG. By considering your lifestyle choices and how the effect these processes, women can take an active role to safeguard their hormonal balance, prevent hormone imbalance, and alleviate health concerns and symptoms.
Hormone Imbalance Testing
A hormone imbalance can lead to various health concerns and symptoms as we’ve discussed. Female hormones like oestradiol, progesterone, FSH, LH, prolactin, free and total testosterone, and SHBG offer insights into reproductive function and potential imbalances6.
Among the available tests, blood tests are essential for measuring these female hormones. These tests help to provide a clear understanding of hormonal health, helping you make informed decisions for a balanced and healthier life6. These tests provide insights that empower informed decisions, nurturing a life marked by balance and vitality.
Randox Health Female Hormone Testing
As part of our Signature, Everywoman, Fertility Health and Female Hormones packages, we test for all the biomarkers discussed in this article and a few others, providing an inclusive assessment of your hormonal health and helping to identify if you may have a hormone imbalance. You can book online, where you’ll be allocated an appointment that suits your schedule.
We are delighted to be able to provide you with the same comprehensive assessment and service from the comfort of your own home. We’ll send you the kit, collect your sample, and send your results within 2-3 days of receiving your sample. A final note however, if your currently taking oral contraceptives, this can affect your results. If you’ve recently stopped taking the pill, it’s best you wait until your periods have returned to normal before booking with us to avoid any false results.
To book your in-clinic or at home female hormones assessment, visit our website or if you’d like any additional information on any of our services, we’d be thrilled to hear from you! Contact us today!
Interested?
We have up to 7 unique health checks centered around women and their hormonal/fertility health including:
- Fertility Health
- Menopause
- Anti-Mullerian Hormone (AMH)
- Polycystic Ovary Syndrome
- Female Hormone
- Blood Borne STI Screen
- Thyroid Health
References
- Mayo Clinic. Estradiol Test.
- Endocrine Society. Reproductive Hormones. https://www.endocrine.org/patient-engagement/endocrine-library/hormones-and-endocrine-function/reproductive-hormones.
- Cable JK, Grider MH. Physiology, Progesterone.; 2023.
- Li RHW, Ng EHY. Serum follicle stimulating hormone to oestradiol ratio as a biomarker for the menopausal transition: a secondary analysis on women in the Study of Women’s Health Across the Nation. Maturitas. 2021;152:67. doi:10.1016/j.maturitas.2021.08.008
- Rieder JK, Darabos K, Weierich MR. Estradiol and Women’s Health: Considering the Role of Estradiol as a Marker in Behavioral Medicine. Int J Behav Med. 2020;27(3):294-304. doi:10.1007/s12529-019-09820-4
- Iino K, Mizunuma H. Biomarkers of Menopause. In: ; 2015:531-543. doi:10.1007/978-94-007-7696-8_9
- Krakowsky Y, Grober ED. Testosterone Deficiency – Establishing A Biochemical Diagnosis. EJIFCC. 2015;26(2):105-113.
- Datta J, Palmer MJ, Tanton C, et al. Prevalence of infertility and help seeking among 15 000 women and men. Human Reproduction. 2016;31(9):2108-2118. doi:10.1093/humrep/dew123
- Sadrzadehh H, Kline G, eds. Endocrine Biomarkers. Elsevier; 2017. doi:10.1016/C2014-0-03865-8
- Wiggs AG, Chandler JK, Aktas A, Sumner SJ, Stewart DA. The Effects of Diet and Exercise on Endogenous Estrogens and Subsequent Breast Cancer Risk in Postmenopausal Women. Front Endocrinol (Lausanne). 2021;12. doi:10.3389/fendo.2021.732255